 A coalition to defend #ourNHS |
||
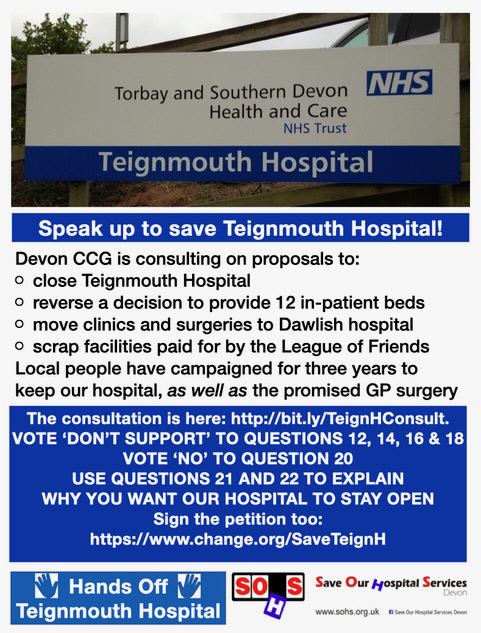 |
Local CampaignsFighting to save Teignmouth HospitalHands Off Teignmouth Hospital and Save Our Hospital Services have produced a response to the public consultation into the proposed closure of Teignmouth Community Hospital. Ignoring a four-year campaign to save the hospital, and strong opposition in earlier consultations, NHS Devon CCG continue to insist that money for a new health and wellbeing centre can only be found if the hospital is closed. We now have evidence that this is not the case. The CCG told us in an email of 10/09/20: 'The construction of the Health and Wellbeing Centre in Teignmouth is not dependent on funds from the sale of the Teignmouth Hospital site.' But minutes of meetings during 2018 show the CCG telling local GPs that they needed to support the 'vision' of closing the hospital in order to open the new centre. Other minutes show the CCG planning to link the two issues during the consultation in order to overcome public opposition to the closure plan. Teignmouth Hospital hosted the community response to COVID-19 in the first wave of infections, providing coordination for health, care and voluntary teams. Closing the hospital would not improve joined-up working. It would reduce the continuity between home and bed-based nursing, as people with complex needs would be sent to a private nursing home and/or out of the area. Teignmouth Hospital provides essential NHS capacity, including many high-use community clinics, specialist clinics, a ward for 12 beds, and a day-care surgical unit. The Dept of Health and Social Care has commanded Trusts and CCGs to make full use of existing capacity to prepare for a second wave of COVID, whether they are nursing acute cases or managing other demands such as community care and elective surgery. Closing the hospital at this time of national health crisis would be madness. Teignmouth Hospital is a much-loved community asset, the first NHS hospital to be purpose built with public funds. Since it was founded in 1954 it has been cherished, maintained, improved, and equipped by the people of Teignmouth, Bishopsteignton and Shaldon, especially through the efforts of the League of Friends. The proposed new-build would be owned a private investment company, leased back to the NHS on a long and expensive PFI lease. We still have no answers on what will happen to all the facilities paid for by local people, including the physiotherapy and occupational therapy suite.  Refurbishing or rebuilding the hospital on the present site has never been fully costed or presented for scrutiny - the only case put forward has been to close it down. The annual (revenue) costs presented in the consultation documents show that for a negligible annual saving (£14k) the locality would lose all the specialist outpatient clinics, surgeries and in-patient capacity of the hospital, and the associated staff and facilities. This comes on top of the closure of the MIU and X-Ray department. It would gain some extra consultation space for community clinics, in a building shared with GPs. This does not seem to local people like a compelling case. The case for closing the hospital rests on a claim that care in people's own homes is more successful than care in a community hospital setting. This case has never been proven. International and UK studies show that home-based care can work if it is funded to at least an equivalent level as hospital care. No assurances have been made that equivalent funding will be put into community nursing teams, to compensate for the loss of capacity at the hospital. We salute the excellent work of community health teams in the locality, but we submit that when bed-based care is required (e.g. for respite, recovery or end-of-life care) it needs to be available within the community, not out of the area or in a private nursing home. A survey by HealthWatch Torbay in January 2020 found that 44% of patients attending the hospital would find the new town centre site more difficult to attend, while 39% would experience 'little or no change'. Meanwhile, moving specialist clinics to Dawlish would cause difficulties for 60% of respondents (23% little or no change). The travel impact document shows that the majority of clinic users will have further to travel, in an area where public transport is poor. These figures are missing from the consultation documents. At present, the CCG's own figures show that the clinics at Teignmouth are treating a far higher number of patients than the equivalent clinics in Dawlish Hospital. Like Newton Abbot - the main beneficiary of earlier service removals - Dawlish is another PFI hospital where clinical space is essentially on lease to the NHS rather than owned by it. We see a pattern across Devon of the CCG promising 'better care' in return for closing 'out of date' hospitals and services, only for these promises to be broken. When Teignmouth's Minor Injuries Unit and X-Ray Department were closed in 2015 it was justified as a new focus on rehabilitation and day surgery. The promised rehabilitation beds did not arrive, and the surgery unit is now to be transferred - at great cost - to Dawlish Hospital. Meanwhile the MIU at Dawlish - supposed to offer a state-of-the-art alternative - has been suspended indefinitely. In just the same way, Dartmouth residents were promised a new health and wellbeing hub and 8 nursing beds when their hospital closed in 2017. The beds were immediately withdrawn, and the proposed new centre - when it is built - will not include any in-patient beds or an X-Ray Department as originally promised. The same pattern has been repeated across Devon. We support the provision of home-based community care, properly funded, and joined up with other health, care and voluntary services. We support investment in primary care. But we object to the loss of 12 community care beds and their nursing capacity from the joined-up care system in the Coastal locality. We object to a further cut in community hospital capacity in an NHS area (Devon) that has already lost 59% of its community beds, with knock-on effects on travel time for vulnerable patients, and on demand for the few remaining facilities. We object to a dependency on nursing beds in private care homes - a sector already struggling under the weight of COVID-19 deaths - for those people with more complex or serious conditions.
For further information please refer to:
|
|
|
Copyright © 2025 Health Campaigns Together
| ||