 A coalition to defend #ourNHS |
||
...Pending a major update...2021
September
July
June
May
March
February
January
2020December
November
October
September
JulyJune
FebruaryJanuaryLong Term Plan2019: Response to NHS England's proposals for new legislationKeep Our NHS Public and HCT have collaborated on this response, the longer version of which has been submitted to NHS England and NHS Improvement's 'engagement process' which concluded on April 25. Also attached is a shorter version developed by KONP.
2018
|
||
 Looking back on Sustainability and Transformation Plans (2016)In many areas old plans for cutbacks and hospital closures were dusted off and rolled out as "new" Sustainability and Transformation Plans during 2016, as a result of instructions issued by NHS England and NHS Improvement on December 23 2015.Most STPs aimed to make huge cash "savings," while NHS funding remained effectively frozen, and set to fall further in real terms till 2020. Many STPs, which were supposed to be implemented by October 2016, hoped to override any accountability or consultation. The plan was to set up new arrangements using delegated powers from trusts, CCGs and local authorities which would put decisions in the hands of a tiny handful of managers - with all of the emphasis from NHS England focused on delivering "savings" to wipe out huge trust deficits. But the plan did not work as NHS England had hoped. In some areas controversial plans were delayed by various factors including action by campaigners, and in many areas there were clear divisions over implementation, with Tory MPs in many areas fearful of the electoral consequences of endorsing cutbacks. Where is no resistance, bad policies can be imposed by unaccountable bureaucrats - doing long-term, possibly permanent damage to our NHS. From early 2016 HCT, through STP Watch, worked to collate and publish resources, links and information as it emerged on what STPs were, how they were supposed to work, and what local services could be at risk. Now the focus has shifted on to Integrated Care Systems, Partnerships and Provider contracts, we have reorganised this information so that the new plans can be compared back to those that were pushed through with such haste and secrecy in 2016. 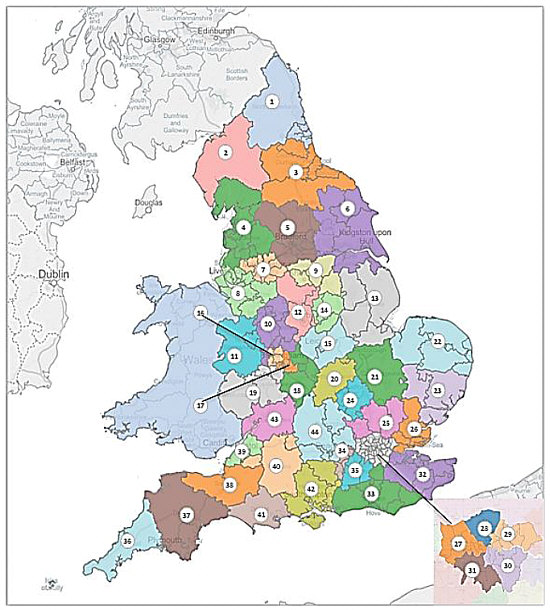 The 44 "Footprints" that cover EnglandThe "footprint" areas in which NHS organisations were required to work together with local government for strategic planning were agreed in a short timescale by local NHS managers early in 2016 - with no consultation whatever with local people or community organisations. Each Footprint has since been required to work as a "local health economy," beginning with drawing up a 1-year plan to restore financial balance, and a 5-Year "Sustainability and Transformation Plan" - supposedly to be finalised by June 2016 - although this was swiftly shown to be impossible.NHS England's full map of the Footprints, with a list so you can find YOUR local Footprint is HERE. Form early 2016 then NHS Improvement boss Jim Mackey and NHS England chief executive Simon Stevens both stressed that this new change is a strategic one, requiring commissioners and providers to collaborate. But even 3 years later, with Lansley's Health & Social Care Act still in force, the hugely expensive and wasteful apparatus of the purchaser-provider split remains. CCGs are still required to put services out to tender - and there is still insufficient funding. Foundation and NHS trusts warned correctly that their deficits were unlikely to be wiped out in 2016-17 - and many are still deep in financial crisis. NHS trust deficitsWhile ministers and NHS England at first demanded NHS trusts must clear deficits before they could receive any of the £1.5 billion "transformation fund", figures from a snap survey of trust board papers in early February 2016 by pressure group London Health Emergency showed trust deficits were bigger than ever, with 138 out of 150 trusts in the red.The total deficits for England's 150 acute trusts were more than a massive £2.2 billion. Just nine trusts were in surplus, sharing a meagre total of £11 million between them. 10 trusts faced deficits of more than £40 million, while three had shortfalls in excess of £70 million, headed by Barts Health, the biggest NHS trust in England, with the biggest debt at a monster £134 million. The STP plansAll 44 STPs were published at the end of 2016, having been endorsed by NHS England despite many of them still being visibly incomplete, with most lacking financial detail, implementation plan and other key elements. They continued to operate behind the scenes.Insofar as they were based on any clear assumptions, most STPs share a common approach of seeking to reduce use of hospital services, reduce hospital provision, and introduce "new models of care". What evidence was there that this approach can work and that new models of care are viable? CLICK HERE for a review by John Lister at the time of the evidence base behind the STPs and the 5-Year Forward View. A list of the published STPs can be found below, by (NHS England allocated) number of STP area (table below), or by geographical area, along with additional relevant documents from that time that help shed light on the obscure process. However even in 2019, some important appendices and documents have either not been published at all, or are no longer accessible online. East
London NCLondon NELondon NW
London SE
London SWMidlands
North East
North West
South
South East
South West
YorkshireCouncil oppositionA number of council leaders and local government bodies spoke out to challenge local STPs, in London, the Midlands, the North West and Yorkshire. In Liverpool the council leader and the Health & Wellbeing Board came out strongly against the Cheshire & Merseyside STP. In London Hammersmith & Fulham council, in alliance with Ealing, committed to a legal challenge to their local STP, which threatened beds and services in Ealing and Charing Cross hospitals. STPs were also rejected by boroughs in SW London and North Central London.A few STP submissions were published early (in October) by local councils (Birmingham, North Central London, South West London, Durham, Darlington, Tees, Hambleton, Richmondshire and Whitby), while a number of even earlier June submissions were also published, some by the NHS and some by local authorities. There's one common factor: health workers and the local public were the last to be informed and only offered "engagement" or token consultation on already final plans as a final gesture before implementation. While the plans were delayed, the pressure for cuts forced the pace of changes that were NOT set out in the STPs. A number of A&E units, maternity and other services in smaller hospitals were closed on "safety" grounds without consultation - indicating the way many of the cutbacks were to be driven through, regardless of the fancy phrases in the STP plans. There was still no public consultation on STP Plans - or even in some cases publication of the proposals - before they were submitted to NHS England and then implemented. Proposed STP governance structures also varied: some set out plans to establish a new leadership bodies such as a "Health & Care Executive", with delegated powers to decide policy and take binding decisions on behalf of all constituent organisations (local NHS commissioners and trusts along with local government). This fitted in with Simon Stevens' clear call for new forms of Combined Authorities that he thought would enable local NHS bosses to "overcome veto power." Hackney CCG shows the weakness of STPs: time to follow suitCity & Hackney Clinical Commissioning Group broke the silence of NHS bodies, to state openly that the STP emperor had no clothes - by insisting, with the support of legal advice that STPs lacked any legal status or powers to compel CCGs or other "partners" to comply with majority decisions.This potentially threw a spanner in the works of all 44 STPs consolidating themselves as bodies to drive controversial cuts, reconfiguration and service changes. Some campaigners and analysts had argued from the beginning that STPs had no legal right to tell any organisation to do anything. And as bodies which function in secret with no transparency or publication of minutes, the STPs have always lacked not only any legal status or statutory role but also any legitimacy or public acceptance. Conservative manifesto promises of plans to change the law to allow STPs to take control had to be scrapped after Theresa May failed to secure a majority in the 2017 General Election. The weakness that remained was powerfully exposed in Hackney, when the CCG has stood out against the plan to merge all 7 NE London CCGs under just one "Accountable Officer" -- a move that would minimise - and effectively avoid - any accountability to local people any of the seven NE London boroughs. Hackney council's Oversight & Scrutiny Committee endorsed this with a powerful letter insisting on the need to retain the statutory levels of accountability that had survived the disastrous 2012 Health & Social Care Act scrapped previous bodies and established CCGs. A Health Service Journal article publicised the CCG's stand. The legal advice sent to the CCG and the letter endorsing the CCG's position and restating clearly the case against local bodies being compelled into collective decisions and losing accountability are all available here.
CCGs give ground in East London StandoffSadly the brave stand taken by City & Hackney CCG was later followed by a climbdown. The local STP (now rebranded as East London Health & Care Partnership (ELHCP) backed up its plan to merge 7 CCGs in North East London into one with a Single Accountable Officer, with the threat of possible funding for "transformation" being withheld of this was not agreed.South Essex STP in chaos as plans to downgrade A&Es are scrappedLocal campaigners were triumphant in 2017 after plans to downgrade A&E services in Southend and Chelmsford's Broomfield Hospital were abandoned by local NHS chiefs.Controversial plans to downgrade two A&E departments in Southend and Chelmsford's Broomfield Hospital were effectively dropped after sustained pressure from campaigners clearly made an impact on local politicians. Local Tory MPs had held on to seats in the June general election, but had clearly pushed behind the scenes soon afterwards to get the plan dropped for fear of further loss of electoral support. During the campaign, angry constituents at a public meeting forced a local Tory MP, Sir David Amess to sign a petition against the downgrading of Southend A&E. What NHS Finance chiefs thought about STPsSTP ResourcesInformation and briefing notes from 2016
Subsequent overviews, Round-ups and analysis
The most complete overview of all 44 STPs was the report published by London South Bank University, and researched by Seán Boyle, John Lister and Roger Steer.In addition to the 85-page general analysis of all the plans, each individual plan was also analysed HERE. 
Whatever Happened to the STPs? by John Lister is a report compiled in June 2018. It was commissioned by UNISON Eastern Region to give members and representatives a realistic analysis of the situation in each STP area.There are six STPs in the region, covering Bedfordshire, Luton & Milton Keynes, Cambridgeshire & Peterborough, Hertfordshire & West Essex, Mid & South Essex, Norfolk & Waveney and Suffolk & NE Essex. Secrecy and obscure language have contributed to public ignorance over STPs, while the documents themselves appeared incomplete and unconvincing from the beginning. However this does not mean that the plans themselves are unimportant. If NHS England had got its way, they would have potentially represented a landmark moment in the development of the NHS in England. This brief survey of what has transpired since the STPs were published at the end of 2016 shows that many of the claims for what STPs might represent and achieve have proved unrealistic. Few have progressed to any extent down the path of genuine collaboration and local partnership. Much of the "integration" that has taken place has in fact been alliances and mergers of commissioners on the one hand and providers on the other - leaving the NHS "purchaser/ provider split" substantially intact. Read or download the full report HERE. National / Background Material
|
||
|
Copyright © 2025 Health Campaigns Together
| ||